Blog
Blogs
Software as a Medical Device (SaMD): What It Is and Why It’s Transforming Healthcare
BLOG by
Software as a Medical Device (SaMD) is redefining how clinical decisions are made, treatments are delivered, and patient outcomes are measured. It represents a class of healthcare software capable of performing medical functions independently of physical hardware. From AI diagnostic platforms to digital therapeutics, SaMD is rapidly becoming a cornerstone of modern healthcare innovation. As regulatory frameworks evolve and machine learning models integrate into clinical workflows, SaMD is emerging not only as a regulatory category but as a transformative force shaping the future of healthcare delivery.
Understanding Software as a Medical Device (SaMD)
The International Medical Device Regulators Forum (IMDRF) defines Software as a Medical Device as software intended to be used for one or more medical purposes that performs these purposes without being part of a hardware medical device. The U.S. Food and Drug Administration (FDA) adopts this definition and evaluates SaMD under its Digital Health framework. In essence, SaMD is standalone software that delivers clinical value, whether diagnosing a disease, recommending treatment, or monitoring a health condition.
Unlike traditional embedded software, SaMD operates independently and can run on cloud systems, smartphones, or clinical networks. Its functionality is validated by medical outcomes rather than by physical integration with a device. Examples include diagnostic algorithms that interpret radiology scans, digital therapy applications that treat mental health conditions, or predictive systems that alert clinicians to potential cardiac events.
According to data published by Orthogonal and FDA consultants, more than 600 SaMD products have received FDA clearance, with estimates suggesting the total active solutions on the U.S. market may range between 700 and 5,000. This rapid expansion highlights the growing confidence in software-driven healthcare systems. The global medical devices market, valued at $518 billion in 2023, is expected to exceed $880 billion by 2032, with SaMD contributing substantially to this growth through its adaptability and scalability.
The IMDRF established the SaMD Working Group in 2013 to create an internationally harmonized framework for risk categorization, quality management, and clinical evaluation. This initiative laid the foundation for global regulatory alignment, enabling both innovation and patient safety. Since then, the FDA, European Commission, Health Canada, and Japan’s PMDA have integrated these principles into their respective approval pathways.
Practical applications of SaMD in healthcare are now visible across multiple domains:
- AI-based imaging software capable of identifying brain lesions or lung nodules with greater precision than manual interpretation.
- Cardiac rhythm monitoring algorithms analyzing continuous ECG data from wearable devices to detect arrhythmias in real time.
- Digital therapeutics platforms like EndeavorRx, which deliver clinically validated interventions for ADHD through an interactive game format.
- Diabetes management applications that recommend insulin doses using data from multiple glucose meters and patient logs.
Each of these examples reflects how software can serve as a medical intervention in its own right. By decoupling clinical intelligence from hardware, SaMD accelerates innovation cycles, reduces costs associated with physical prototyping, and allows continuous refinement through real-world performance data.
The Rise of Software-Driven Healthcare
The evolution of Software as a Medical Device (SaMD) reflects a broader transformation across healthcare, where software intelligence increasingly defines clinical precision, accessibility, and outcomes. Over the last two decades, medical devices have transitioned from static, hardware-centric systems to adaptive, data-driven platforms capable of continuous learning and feedback. This shift has allowed software to move from a supporting element of care to a primary clinical asset.
According to the World Health Organization’s MeDevIS platform, more than 10,000 medical devices are currently in use worldwide for prevention, diagnosis, and treatment. A growing proportion of these devices now rely on software-based functions that enable automation, connectivity, and analytics. The emergence of the Internet of Things (IoT), cloud infrastructure, and artificial intelligence has accelerated this evolution, creating medical ecosystems where software applications interact directly with patients, clinicians, and health systems.
A clear measure of this transformation can be seen in the expansion of AI and machine learning-enabled medical devices. As of mid-2024, the FDA had authorized over 950 AI or ML-enabled medical devices, up from just 64 in 2018. Many of these products qualify as SaMD, offering capabilities that include diagnostic imaging, predictive analytics, and personalized treatment recommendations. The acceleration of approvals underscores both the regulatory maturity and clinical acceptance of software-based care models.
In practice, SaMD is reshaping three critical areas of healthcare delivery:
- Diagnostics and Early Detection
Software algorithms now analyze complex imaging and physiological data faster and more accurately than traditional methods. AI-driven diagnostic platforms such as EchoGo assist cardiologists in detecting heart failure and coronary artery disease from echocardiograms with over 90 percent accuracy, shortening the time between symptom presentation and treatment initiation. - Remote Monitoring and Preventive Care
Connected applications process data from wearable biosensors to provide clinicians with real-time insights into patient health. Solutions such as physIQ map dynamic baselines of vital signs, identifying deviations that signal potential deterioration long before clinical symptoms become visible. This continuous monitoring reduces hospital readmissions and improves chronic disease management. - Digital Therapeutics and Behavioral Health
Software-delivered interventions are now used for conditions ranging from insomnia to attention disorders. EndeavorRx, for example, became the first FDA-cleared digital therapeutic for ADHD, demonstrating that clinically validated software can serve as a standalone treatment. Similarly, platforms like Regulora offer digital hypnotherapy for irritable bowel syndrome, expanding access to proven behavioral therapies beyond clinical settings.
These examples illustrate how SaMD extends healthcare beyond hospital walls, aligning with the global shift toward patient-centric and value-based care. The integration of continuous data capture, intelligent analytics, and interoperable platforms allows healthcare providers to move from episodic treatment to proactive management. For patients, this means earlier interventions, personalized therapies, and greater engagement in their own care journey.
As SaMD adoption accelerates, healthcare organizations increasingly view software as a strategic investment rather than an adjunct to hardware. This shift marks the beginning of a software-defined era in healthcare, one where algorithms, not instruments, drive the next wave of medical innovation.
Key Characteristics of Software as a Medical Device (SaMD)
The defining strength of Software as a Medical Device lies in its ability to deliver medical value independently across multiple computing environments without reliance on proprietary hardware. While its scope varies by clinical application, every SaMD solution shares foundational characteristics that distinguish it from other forms of medical software.
- Independent Clinical Functionality
A SaMD performs a diagnostic, therapeutic, or preventive function on its own. Its clinical impact is derived from its algorithmic capability rather than physical components. For example, an AI-powered ophthalmology application that analyzes retinal scans to detect early signs of diabetic retinopathy qualifies as SaMD even when used on a standard mobile or desktop device. - Platform Agnostic Deployment
Because SaMD operates independently of dedicated hardware, it can be deployed across cloud systems, smartphones, tablets, or hospital servers. This adaptability makes it scalable and cost-efficient for healthcare providers. Cloud-based architectures also allow seamless updates, version control, and real-world data integration, features that traditional hardware devices cannot achieve without physical modification. - Medical Purpose and Patient Risk Relevance
Each SaMD is defined by its intended medical purpose. It must contribute directly to diagnosing, treating, mitigating, or preventing disease. This purpose determines its regulatory classification and risk category. For instance, a wellness application that tracks heart rate trends without diagnostic interpretation is not SaMD, whereas a cardiac monitoring app that identifies arrhythmias based on ECG data is. - Data-Driven Intelligence
SaMD leverages large-scale data inputs to enable precise medical decisions. These data sources include imaging repositories, wearable sensors, laboratory systems, and patient-reported outcomes. Real-time analytics, machine learning models, and predictive algorithms transform this information into actionable insights. As a result, clinicians can make faster and more informed decisions while patients benefit from early detection and personalized care. - Continuous Learning and Iteration
Unlike conventional medical devices that undergo fixed approval cycles, SaMD evolves continuously through software updates and post-market performance monitoring. Modern regulatory programs such as the FDA’s Predetermined Change Control Plan (PCCP) framework support this evolution by allowing predefined algorithm updates without requiring full resubmission. This approach enables developers to refine diagnostic accuracy or adapt to new data while maintaining compliance. - Interoperability Across Clinical Systems
To function within real-world healthcare environments, SaMD must integrate with electronic health records (EHRs), diagnostic imaging systems, and cloud-based care coordination platforms. Compliance with interoperability standards such as HL7, FHIR, and DICOM ensures that SaMD solutions exchange data securely and consistently across institutions and geographies. - Quality and Regulatory Alignment
Every SaMD must conform to quality management systems aligned with ISO 13485, as well as cybersecurity, privacy, and usability standards. Regulatory oversight extends from initial risk analysis to post-market surveillance, ensuring that patient safety is never compromised throughout the software’s lifecycle.
Collectively, these characteristics define why SaMD represents a distinct class of medical innovation. It combines the rigor of traditional medical device regulation with the agility of modern software engineering. By integrating artificial intelligence, real-time data analytics, and interoperable design, SaMD redefines what healthcare systems can achieve without dependency on physical instrumentation.
SaMD vs Other Types of Medical Software
Software as a Medical Device is often misunderstood as a broad term that includes all forms of healthcare software, but it holds a specific regulatory and clinical distinction. To understand its scope, it is essential to differentiate SaMD from other categories of medical software recognized by global regulators such as the FDA and the International Medical Device Regulators Forum (IMDRF).
- Software in a Medical Device (SiMD)
This refers to software that is an integral part of a physical medical device. It is embedded in the hardware and directly controls or operates it. Examples include firmware that manages the pacing algorithm in a pacemaker or the control software used in an MRI scanner. The software and hardware together form one regulated medical device.
- Software as a Medical Device (SaMD)
Unlike SiMD, SaMD performs its medical function independently. It does not require dedicated hardware and is validated based on its software functionality and clinical effectiveness. A cardiac rhythm analysis application that detects arrhythmias or a diagnostic imaging algorithm that identifies tumors from radiology scans are examples of SaMD. These applications are platform agnostic and can be deployed on mobile devices, tablets, or cloud environments.
- Accessory Software
Accessory software supports a medical device but does not perform a direct medical function. For example, an app that allows clinicians to remotely adjust the settings of an insulin pump is considered accessory software. It enables convenience and usability but does not diagnose or treat medical conditions.
- Health and Wellness Applications
These are consumer-grade software products that help users monitor general wellness indicators such as fitness, sleep, or diet. They are not subject to the same regulatory standards as SaMD because they do not provide diagnostic or therapeutic outputs. A step-counting app or a sleep-tracking tool are common examples.
Comparison Overview
Type | Purpose | Dependency on Hardware | Regulatory Oversight | Example |
SaMD | Diagnoses, treats, or prevents disease | Independent | Strict (FDA, IMDRF, MDR) | AI radiology software, diabetes management app |
SiMD | Operates a physical medical device | Dependent | Strict (FDA, CE, ISO) | Pacemaker firmware, ventilator control software |
Accessory Software | Supports a medical device | Dependent | Moderate | Remote control app for imaging device |
Wellness App | Tracks fitness or lifestyle | Independent | Minimal | Step counter, sleep tracker |
Understanding these distinctions helps healthcare organizations, developers, and regulators align expectations and compliance pathways. SaMD uniquely stands apart because it delivers medical value through software intelligence rather than through a hardware-driven mechanism. It can analyze, predict, or recommend clinical actions autonomously, transforming software into a primary medical tool rather than a supportive one.
As global adoption increases, clear categorization is vital to ensure safety, transparency, and consistent regulation. For technology partners and healthcare innovators, recognizing where their product falls within these categories determines the required validation, documentation, and regulatory strategy.
Regulatory Foundations for Software as a Medical Device (SaMD)
The regulation of Software as a Medical Device is built on global frameworks designed to balance innovation with patient safety. Unlike consumer or enterprise software, SaMD is classified as a medical product and therefore must comply with rigorous regulatory standards that govern its development, validation, and ongoing performance.
The International Medical Device Regulators Forum (IMDRF) established the first harmonized global framework for SaMD in 2013. The IMDRF defined key principles covering risk categorization, quality management, and clinical evaluation. These principles are now used by the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), Health Canada, Japan’s PMDA, and other national authorities to create consistent pathways for software regulation.
Global Alignment Through IMDRF and FDA
The IMDRF defines SaMD as software that performs a medical purpose on its own. This definition forms the foundation of the FDA’s approach, which classifies SaMD as a medical device under the Federal Food, Drug, and Cosmetic Act. The FDA evaluates SaMD submissions based on safety, effectiveness, and risk.
Depending on the intended use and level of clinical risk, SaMD is placed into regulatory classes similar to traditional medical devices:
- Class I: Low-risk software such as wellness monitoring tools or symptom trackers used for general health guidance.
- Class II: Moderate-risk products, including diagnostic support software that assists but does not replace a clinician’s decision.
- Class III: High-risk software that performs critical medical functions such as life support or autonomous diagnosis.
The FDA’s Digital Health Center of Excellence provides detailed guidance on the submission and approval of SaMD products. It outlines requirements for software validation, data management, and cybersecurity. Over the last five years, the FDA has accelerated approvals for AI-driven SaMD products, including adaptive algorithms used for imaging diagnostics, cardiology, and endocrinology.
European Union and Global Regulatory Standards
In Europe, SaMD falls under the Medical Device Regulation (MDR) framework, which mandates compliance with ISO 13485 quality management systems. The MDR also requires a clinical evaluation process similar to FDA requirements, ensuring that SaMD products demonstrate safety, accuracy, and reproducibility. Other major regions, including Canada and Australia, follow comparable guidelines based on the IMDRF model, using national equivalents such as the Canadian Medical Device Regulations (CMDR) and the Therapeutic Goods Administration (TGA) standards.
Risk Categorization and Quality Management
Risk classification determines the depth of validation, documentation, and post-market monitoring required. High-risk SaMD must undergo clinical evaluation, verification testing, and human factors validation. ISO 13485 remains the global benchmark for ensuring that the development process meets traceability, documentation, and design control standards.
Many SaMD developers also adopt ISO 14971, the international standard for risk management in medical devices. This framework ensures that every possible hazard, from algorithmic error to cybersecurity vulnerability, is identified, analyzed, and mitigated throughout the software lifecycle.
Clinical Evaluation and Post-Market Oversight
For a SaMD to obtain regulatory clearance, it must demonstrate clinical validity and performance through evidence-based testing. Developers are required to conduct both analytical validation, which verifies software accuracy, and clinical validation, which confirms its real-world effectiveness. Post-market surveillance is equally important. Continuous monitoring allows developers to collect data on performance, detect anomalies, and apply updates safely through controlled processes such as the FDA’s Predetermined Change Control Plan (PCCP).
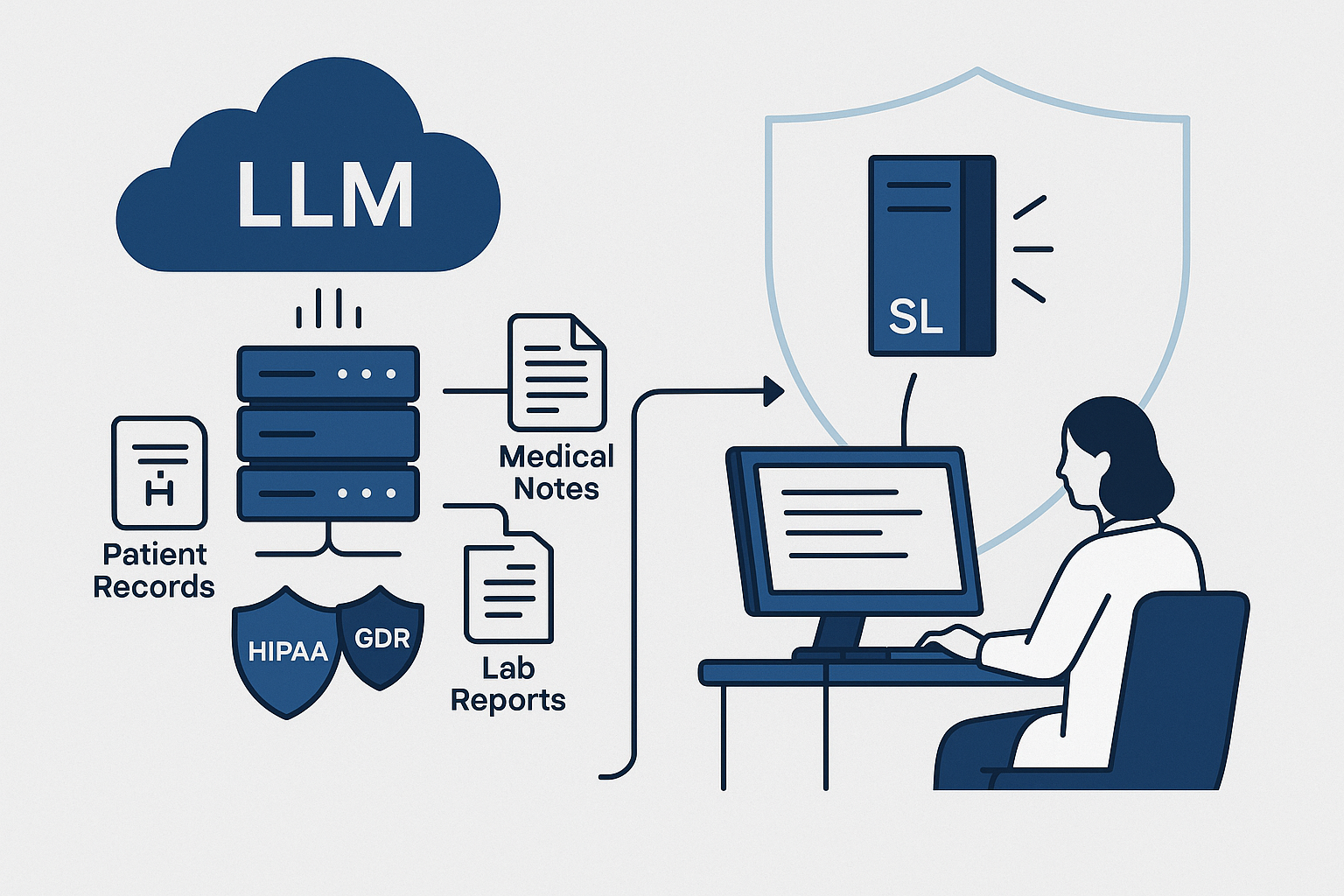
Data Privacy and Security Compliance
In addition to regulatory approval, SaMD must comply with privacy and security laws. In the United States, this includes the Health Insurance Portability and Accountability Act (HIPAA) and the Health Information Technology for Economic and Clinical Health Act (HITECH). In Europe, compliance with the General Data Protection Regulation (GDPR) ensures that patient data is handled with transparency and integrity. Developers must implement encryption, access control, audit trails, and intrusion prevention systems to maintain compliance across jurisdictions.
Collectively, these regulatory frameworks provide the foundation for safe and effective SaMD innovation. By enforcing transparency, quality, and accountability, they enable developers and healthcare organizations to deliver clinically trusted digital solutions that meet the same standards as traditional medical devices.
How Software as a Medical Device (SaMD) Is Transforming Patient Care
The widespread adoption of Software as a Medical Device has begun to reshape the way healthcare is delivered, measured, and experienced. Unlike traditional medical devices that rely on physical mechanisms, SaMD harnesses data, intelligence, and connectivity to enable continuous, adaptive, and evidence-based care. Its impact can already be seen in diagnostics, chronic disease management, preventive care, and patient engagement.
Enhancing Diagnostic Accuracy
SaMD applications have proven especially valuable in diagnostic imaging, where speed and precision are critical. Machine learning algorithms now assist radiologists in detecting subtle abnormalities in scans that may be missed through manual review. For example, the EchoGo platform, cleared by the FDA, analyzes echocardiogram images to identify heart failure and coronary artery disease with accuracy exceeding 90 percent. Similar AI-driven diagnostic systems for dermatology, ophthalmology, and neurology are improving early detection rates and reducing the time between imaging and intervention.
Enabling Real-Time Monitoring and Predictive Care
SaMD enables clinicians to monitor patients remotely using data captured through wearable or implanted sensors. These applications analyze physiological signals such as heart rate variability, oxygen saturation, and blood pressure to identify risk patterns before they lead to acute events. The physIQ analytics system provides a proven example of this capability. It processes multiple vital signs from wearable biosensors to create a personalized baseline and detect deviations that may indicate disease progression. This approach supports proactive care and significantly reduces hospital readmissions among patients with chronic conditions.
Advancing Digital Therapeutics and Personalized Treatment
Digital therapeutics, a major subset of SaMD, have demonstrated clinical efficacy in managing neurological, metabolic, and behavioral health disorders. EndeavorRx, the first FDA-approved prescription video game, is used to treat ADHD by improving attention control in children through adaptive sensory engagement. Similarly, Regulora delivers digital hypnotherapy for patients with irritable bowel syndrome, providing access to treatment previously limited to specialized clinics. These software-based interventions expand the reach of therapy while maintaining clinical supervision and evidence-based validation.
Reducing Diagnostic and Treatment Delays
Traditional diagnostics often depend on in-person visits and lab processing times, which can delay treatment initiation. SaMD reduces these barriers by allowing immediate analysis and actionable results. In oncology and cardiovascular care, algorithms can now identify high-risk findings within minutes, prompting earlier medical response. By shortening diagnostic cycles, SaMD helps improve survival rates and optimize resource allocation for healthcare systems.
Improving Accessibility and Affordability of Care
By removing the dependency on specialized hardware and clinical infrastructure, SaMD expands access to healthcare services in underserved or remote areas. Cloud-based platforms allow patients and providers to interact through secure mobile applications, enabling monitoring and consultation outside hospital settings. This model supports the global shift toward home-based and preventive care. It also reduces operational costs for healthcare organizations while increasing patient satisfaction and adherence to treatment.
Driving a Shift Toward Continuous and Preventive Care Models
The traditional healthcare model focuses on episodic treatment, often triggered by acute symptoms. SaMD reverses this paradigm by enabling continuous data collection and longitudinal patient insights. This allows healthcare providers to identify early warning signs, measure treatment response, and make data-backed decisions over time. The result is a transition toward preventive and personalized care where outcomes are measured by health improvement rather than volume of procedures.
Empowering Patients Through Engagement and Data Ownership
SaMD enhances patient engagement by giving individuals direct access to health data and personalized insights. Through interactive interfaces and actionable alerts, patients gain a clearer understanding of their conditions and the steps required to maintain stability. This empowerment fosters stronger collaboration between patients and clinicians, leading to higher adherence rates and better long-term outcomes.
Software as a Medical Device is no longer an experimental concept. It is a clinical reality that enables precision, scalability, and accessibility across the continuum of care. As adoption continues to grow, the relationship between patients, providers, and technology will evolve into a unified ecosystem built on continuous insight and measurable health impact.
Emerging Trends Shaping Software as a Medical Device (SaMD)
The landscape of Software as a Medical Device continues to evolve rapidly, driven by technological progress, regulatory innovation, and growing clinical trust in digital tools. These trends are expanding SaMD’s capabilities from diagnostic assistance to autonomous decision support and preventive healthcare.
Artificial Intelligence and Machine Learning Integration
AI and machine learning are transforming SaMD into adaptive systems capable of learning from real-world data. Algorithms can now process millions of imaging or physiological data points to improve accuracy over time. The FDA has already authorized more than 950 AI or ML-enabled medical devices, a number that has nearly doubled since 2021. This reflects a global acceptance of intelligent software that supports clinicians in decision-making and enables predictive healthcare.
Emerging regulatory mechanisms such as the Predetermined Change Control Plan (PCCP) allow developers to update algorithms without reapplying for full FDA clearance, provided that the modifications fall within predefined safety and performance boundaries. This approach supports iterative improvement while maintaining transparency and oversight.
Expansion of Cloud and Edge Computing in SaMD
Modern SaMD applications increasingly rely on distributed computing models to handle large volumes of healthcare data. Cloud platforms enable seamless access, while edge computing allows local data processing on connected devices for faster response times and reduced latency. In clinical practice, this means diagnostic models can analyze imaging data directly on a scanner or wearable device while synchronizing results to cloud systems for long-term tracking.
Interoperability and Data Exchange
Interoperability is becoming a cornerstone of SaMD development. Adoption of standards such as HL7 FHIR and DICOM ensures that SaMD products can integrate seamlessly with electronic health records, laboratory information systems, and telehealth platforms. This integration promotes unified clinical workflows and eliminates data silos. Interoperable SaMD solutions enable clinicians to view comprehensive patient data across multiple systems, improving coordination and diagnostic accuracy.
Cybersecurity and Data Governance
The digital nature of SaMD requires continuous attention to security. In 2023, the FDA issued updated guidance on cybersecurity for medical devices, mandating built-in safeguards such as authentication, access control, and data encryption. Compliance with frameworks like HIPAA, GDPR, and ISO 27001 is no longer optional but a baseline expectation. Secure design principles and ongoing threat monitoring protect both patient data and clinical integrity.
SaMD as a Driver of Precision and Personalized Medicine
By combining AI, real-time analytics, and interoperable data, SaMD is enabling highly personalized treatment paths. These systems analyze genetic, behavioral, and environmental data to tailor therapies for individual patients. Precision oncology, digital neurotherapy, and metabolic disease management are among the fastest-growing areas where SaMD is directly influencing clinical decision-making.
Common Challenges in SaMD Development
While the potential of Software as a Medical Device is significant, developing a clinically validated, compliant, and scalable product requires overcoming several operational and regulatory challenges.
Balancing Agility with Regulatory Compliance
Healthcare software must evolve quickly to meet patient and market needs, but medical device regulation demands rigorous documentation and validation. Maintaining an agile development model within a regulatory framework requires disciplined processes. Companies that integrate compliance into early design stages, rather than treating it as a final checkpoint, achieve faster regulatory approval and smoother audits.
Ensuring Data Accuracy and Model Transparency
The effectiveness of SaMD depends on the reliability of the data that powers it. Inaccurate or biased datasets can compromise diagnostic or therapeutic accuracy. Regulatory bodies increasingly emphasize explainability in AI-driven SaMD to ensure that clinical decisions derived from algorithms can be interpreted and justified by healthcare professionals.
Interoperability and System Integration
Integrating SaMD into existing healthcare infrastructure can be complex. Hospitals and clinics often operate multiple legacy systems with limited compatibility. Meeting interoperability requirements through FHIR, DICOM, and secure API integrations is essential to ensure seamless data flow and compliance with regulatory expectations.
Cybersecurity and Patient Trust
Cybersecurity risks pose one of the greatest challenges to SaMD adoption. Breaches or data manipulation can endanger patient safety. The FDA now expects manufacturers to implement real-time threat detection, encryption, and secure software update mechanisms. A strong cybersecurity posture directly correlates with patient and provider trust.
Validation and Real-World Evidence
Clinical validation remains a cornerstone of SaMD approval. Demonstrating performance consistency across diverse populations and healthcare settings requires extensive testing and post-market surveillance. Developers are now leveraging real-world evidence and continuous monitoring systems to maintain regulatory compliance and improve model performance.
The Future of Software as a Medical Device in Healthcare Innovation
SaMD represents more than a digital adaptation of existing medical devices; it signifies a foundational shift toward data-centric healthcare ecosystems. The convergence of cloud computing, AI, and regulatory innovation is creating conditions for a new generation of adaptive, intelligent medical software.
Over the next decade, SaMD is expected to play a decisive role in:
- Predictive medicine, where algorithms anticipate disease risk and recommend interventions before symptoms emerge.
- Autonomous clinical decision support, assisting physicians with precision-level diagnostics.
- Digital therapeutics, where software itself becomes a clinically prescribed treatment for conditions like depression, chronic pain, or neurological disorders.
Market forecasts from Fortune Business Insights project the global medical device sector to surpass $880 billion by 2032, with software-defined devices contributing a major share of that growth. As clinical validation frameworks become standardized, SaMD will extend into specialized fields such as mental health, ophthalmology, and rehabilitation, where digital interfaces can deliver continuous therapeutic value.
The future of SaMD lies in integration rather than isolation. It will connect patients, providers, payers, and systems through intelligent, compliant platforms capable of evolving alongside medical science. As healthcare organizations invest in digital transformation, SaMD will form the technological foundation for precision, personalization, and preventive care worldwide.
Partnering with Experts to Build the Next Generation of SaMD
Developing a compliant and clinically validated Software as a Medical Device requires deep expertise in both technology and healthcare regulation. Success depends on more than programming skill; it demands an understanding of clinical workflows, data integrity, and international compliance frameworks.
CitrusBits partners with healthcare innovators, providers, and life sciences organizations to design and develop enterprise-grade SaMD solutions that meet the highest standards of performance and safety. Through its Build, Protect, Operate, and Innovate model, CitrusBits ensures that every solution is engineered with compliance, scalability, and patient impact in mind.
- Build focuses on strategy, design, and platform architecture, creating reliable and intuitive medical-grade software.
- Protect embeds HIPAA, FDA, CE, and ISO 13485 compliance into every phase of development.
- Operate delivers continuous support, lifecycle management, and platform optimization.
- Innovate integrates artificial intelligence, interoperability, and emerging technologies to future-proof solutions.
CitrusBits has contributed to healthcare projects involving AI-based diagnostics, XR-powered clinical training, and data-driven digital health platforms. Its expertise in regulated healthcare environments enables clients to accelerate development without compromising compliance or quality.
As Software as a Medical Device continues to redefine healthcare, partnerships between innovators and experienced technology providers will determine which organizations lead this transformation. Working with a trusted development partner ensures not only regulatory readiness but also the ability to deliver measurable improvements in patient outcomes and operational efficiency.
About the Author
Content Writer
Related blogs
BLOG
BLOG